
General Dentistry
We at Picnic Point Dental Clinic offer variety of General Dental services to our patients, These include:
1) Examination & Consultations
2) Check-up & Clean
3) Restorative Fillings
4) Periodontal Therapy
5) Endodontic Therapy (Root Canal therapy)
6) Teeth Extractions, Wisdom Teeth & Oral Surgery
7) Teeth Grinding & Chipping
8) Dentures
9) Mouthguards & Sportsguards

Examination & Consultation
What to expect at your first appointment?
Upon your first appointment or consultation, Dr Carter will gather a very detailed Medical & Dental history of every patient, he will listen to your concerns/ problems and try to find out solutions and treatment options that matches your desire and wants.
Then, Dr Carter will carry his through clinical examination and assess every individual patient’s oral health. Dr Carter will use the latest technologies available in evidence based-dentistry today in detecting dental caries/decay and periodontal/gum disease these include but not limited to magnifying dental microscopes, digital radiographs, intraoral camera, LEDEX Caries detection technology and Perio POC Pro the most sophisticated device in periodontal diagnostics from GenSpeed international. Dr Carter will use these tools during the initial diagnostic examination appointment to correctly diagnose what sort of problem do you have. He will discuss with you the findings along with the treatment options in a simple and easy to understand manner. Dr Carter will discuss with you all the pros and cons of different treatment options and at the end will tailor a defined treatment plan that you agree with.
Call us today to make an appointment and experience the difference.
Check-ups & Clean
Regular dental check-ups and clean are very important for long term oral, general health and wellbeing.
At Picnic Point Dental Clinic we strongly believe that prevention is always better than cure, this is why we stress the importance of your preventative care appointment and regular dental check-ups and hygiene. Coming to see us every 6 months will help catch any signs of early decay, gum disease or any other oral health problems that may become a bigger issue in the future, if left untreated.
As part of your initial check-up, we recommend 2 standard x-rays to check in between your teeth. This is a very important part of your dental hygiene routine, as sometimes it is not possible to check in between your teeth and under any old fillings or crowns that could possibly have decay underneath them.
Brushing morning and night and daily flossing, together with good oral hygiene practice and regular dental check-ups, should help prevent the need for fillings and any further restorations in the future. You are also decreasing the risk of developing gum disease and other dental problems, and ensuring a healthy mouth and smile.
Call us today to make an appointment and experience the difference.

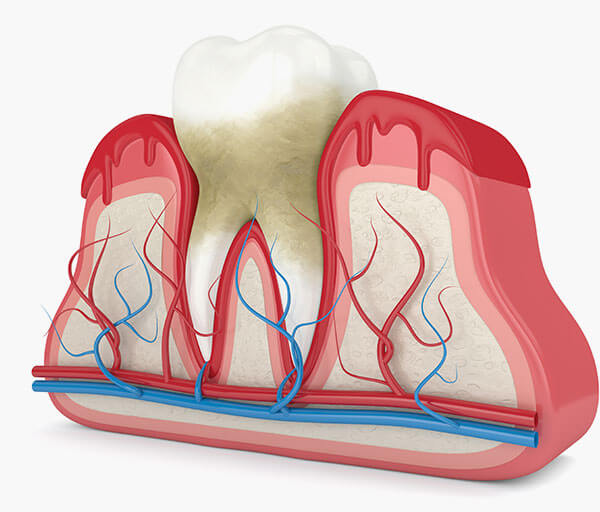
Periodontal Therapy (Gum Treatment)
Fifty percent of people aged over 40 years suffer from periodontitis (gum disease). Despite those numbers that mark periodontitis as one of the most common infectious diseases it is widely neglected. Often painless gum disease can remain symptom-less or you may notice bleeding gums, bad breath, gum recession, swollen gums and sensitive teeth. Thousands of bacteria live in our mouths. Most are harmless, but some release toxins which cause damage to the supporting structures of our teeth.
Gum disease is caused by bacteria that form a biofilm commonly called plaque around the teeth when they are not cleaned properly. The bacteria cause bleeding, infection and inflammation. A bad taste may develop along with bad breath (or halitosis). Gum disease or gingivitis can eventually lead to loose teeth and in some cases abscesses.
Dr Carter utilises a state- of the art diagnostic device in detecting periodontal/gum disease. Its called Perio POC Pro from GenSpeed GmbH.
It is the only chairside test available in Australia to detect Periodontal pathogens. This is a breakthrough technology and only available at Picnic Point Dental Clinics & Sydney Southwest Implant Centre.
PerioPOC® at a glance:
- Microbial chair-side test for periodontitis and peri-implantitis
- Time to result 20 minutes
- No shipment of patient samples
- No laboratory equipment required
- Detects only living bacteria – no false positives
PerioPOC and the new automated PerioPOC Pro enable Dr Carter to obtain reliable results within a few minutes. All patients at risk for periodontitis or peri-implantitis will profit form this state-of-the-art service.
Following a comprehensive dental examination Dr Carter will work together to provide treatment plan such as full mouth detox or specific periodontal therapy (non-surgical & Surgical).
Gum disease is highly complex, infectious and progressive and if left untreated can lead to tooth loss.
If you ever suffered or currently suffering of any of the following symptoms:
- Inflamed bleeding gums
- Sensitive teeth
- Bad breath (halitosis)
- Dry mouth
- Gum recession & uneven gum lines,
- Tender tooth to eat/bite
- Bad taste
- Loose tooth/teeth
Make an appointment to day to check if you have the Periodontal pathogens that causes gum disease.
Untreated Gum/Periodontal disease is a considered a risk factor for more serious cardiovascular disease, Diabetes, Dementia & Alzheimer’s and infertility in women!
Call us today to make an appointment and experience the difference.
Restorative Fillings
Picnic Point Dental Clinic (PPDC) is an amalgam-free practice. We only use white tooth-coloured materials to restore the teeth.
Fillings are necessary when you have developed a cavity, a piece of tooth has broken, or an existing filling requires replacement. our clinical team only uses white tooth-coloured materials to restore your teeth making the fillings practically undetectable. Composite resin is reliable, durable and visually pleasing than old amalgam material.
Over time the technology for tooth-coloured fillings has improved greatly, providing longevity and a great aesthetic result. We can also replace any old ugly amalgam fillings that may have cracked or decayed, with a new tooth coloured filling.
For larger restorations and replacement of big, old amalgam fillings, composite resin is unlikely to be a sufficient long-term option. In these cases, porcelain (inlay/onlay) are the ideal course of treatment. Preventative 6 monthly dental check-ups are the best way to avoid the need for fillings. By detecting tooth decay early and acting, you avoid more extensive (and expensive) treatment.
Tooth decay doesn’t hurt, but once it’s present it only gets bigger.
Call us today to make an appointment and experience the difference.

Endodontics & Root Canal Therapy
At Picnic Point Dental Clinic (PPDC) our mission is to save teeth for patients. Root canal therapy allows us to save infected or heavily decayed teeth, which would otherwise need tooth extraction. We believe there is nothing better than your own teeth. That is why we place such emphasis on trying to save and restore them. If the tooth can be saved by undergoing root canal therapy, it’s a worthy investment in yourself! Root canal treatment is a very delicate process and must be completed to ensure the tooth doesn’t become inflamed (re-inflamed) or infected (reinfected). Nothing is ever as good as the original teeth you were born with!
Is Root Canal Therapy Painful?
Root canal treatment is PAIN FREE, there is nothing to be afraid of! Root canal therapy is needed if decay has spread to the tooth nerve (pulp chamber), or if a crack has developed down into the root of the tooth. Root canal therapy is done over a number of visits, depending on the reason for having the treatment.
Our clinical team will use the latest technology in assessing teeth for Root canal Therapy. Upon assessment completion our clinical team will discuss prognosis of such treatment for the tooth and whether it’s worth investing in or not. If our clinical team recommends RCT it can be done either in one-visit technique or multiple visits technique based on every individual patient case.
Then the following steps and appointments are required:
Visit 1: The tooth is first cleaned from caries, infection and dead nerve tissue and medicated to alleviate symptoms along with a temporary filling.
Visit 2: Once our clinical team is satisfied the tooth has settled, they will then commence cleaning, reshaping the canals, and place new medication in the tooth. Our clinical team will only use rotary nickel titanium files on a specialised electronic appliance to give you the best root canal possible. Our clinical team will use our Dental Magnifying microscope along with our Sophisticated EndoPilot Device to prepare the tooth (the only clinic in Southwest Sydney to use such technology). This process allows us to shape the canal(s) to make them suitable for the custom fitted root filling material (called Gutta Percha).
Visit 3: At the final root canal therapy appointment, our clinical team will insert a custom fitted root filling material (Gutta Percha) to stabilise the tooth and prevent microleakage using the latest technologies available in Endodontics.
Visit 4: For best long-term prognosis, the tooth is then covered with a permanent filling or a dental crown to give maximum strength. A porcelain crown is recommended to protect the tooth from further deterioration or breakage.
This process commonly requires 2-3 visits, although more visits may be required depending on each patient’s needs.
In certain circumstances where there may be a complex canal shape or difficulty in accessing the canals due to the age or condition of the tooth, we will refer you to our local specialist. With their report an informed decision can be made on the long-term outcome for the tooth or teeth involved.
Call us today to make an appointment and experience the difference.
Wisdom teeth & Oral Surgery/ Extractions
Patients should know that whatever your oral needs, from the first consultation through to post treatment recovery, we’ll be with you every step of the way. Our clinical team includes a highly experienced Dental Surgeon that can help with simple or complex wisdom teeth removal procedures.
Overview of wisdom teeth Extraction
Wisdom tooth extraction is a surgical procedure to remove one or more wisdom teeth — the four permanent adult teeth located at the back corners of your mouth on the top and bottom.
If a wisdom tooth doesn’t have room to grow (impacted wisdom tooth), resulting in pain, infection or other dental problems, you’ll likely need to have it removed.
To prevent potential future problems, some dentists and oral surgeons recommend wisdom tooth extraction even if impacted teeth aren’t currently causing problems.
Why do we need to do it?
Impacted wisdom teeth
Wisdom teeth, or third molars, are the last permanent teeth to appear (erupt) in the mouth. These teeth usually appear between the ages of 17 and 25. Some people never develop wisdom teeth. For others, wisdom teeth erupt normally — just as their other molars did — and cause no problems.
Many people develop impacted wisdom teeth — teeth that don’t have enough room to erupt into the mouth or develop normally. Impacted wisdom teeth may erupt only partially or not at all.
An impacted wisdom tooth may:
- Grow at an angle toward the next tooth (second molar)
- Grow at an angle toward the back of the mouth
- Grow at a right angle to the other teeth, as if the wisdom tooth is “lying down” within the jawbone
- Grow straight up or down like other teeth but stay trapped within the jawbone
Problems with impacted wisdom teeth
You’ll likely need your impacted wisdom tooth removed if it results in problems such as:
- Pain
- Trapping food and debris behind the wisdom tooth
- Infection or gum disease (periodontal disease)
- Tooth decay in a partially erupted wisdom tooth
- Damage to a nearby tooth or surrounding bone
- Development of a fluid-filled sac (cyst) around the wisdom tooth
- Complications with orthodontic treatments to straighten other teeth
Preventing future dental problems
Dental specialists disagree about the value of extracting impacted wisdom teeth that aren’t causing problems (asymptomatic).
It’s difficult to predict future problems with impacted wisdom teeth. However, here’s the rationale for preventive extraction:
- Symptom-free wisdom teeth could still harbor disease.
- If there isn’t enough space for the tooth to erupt, it’s often hard to get to it and clean it properly.
- Serious complications with wisdom teeth happen less often in younger adults.
- Older adults may experience difficulty with surgery and complications after surgery.
Request an Appointment at Picnic Point Dental Clinic
Risks
Most wisdom tooth extractions don’t result in long-term complications. However, removal of impacted wisdom teeth occasionally requires a surgical approach that involves making an incision in the gum tissue and removing bone. Rarely, complications can include:
- Painful dry socket, or exposure of bone when the post-surgical blood clot is lost from the site of the surgical wound (socket)
- Infection in the socket from bacteria or trapped food particles
- Damage to nearby teeth, nerves, jawbone or sinuses
How you prepare
Our clinical team may perform the procedure in the office. However, if your tooth is deeply impacted or if the extraction requires an in-depth surgical approach, our clinical team may suggest you see an oral surgeon. In addition to making the area numb with local anesthetic, our clinical team may suggest sedation to allow you to be more comfortable during the procedure.
Questions to ask
Questions you may want to ask our clinical team include:
- How many wisdom teeth need to be removed?
- What type of anesthesia will I receive?
- How complicated do you expect the procedure to be?
- How long is the procedure likely to last?
- Have the impacted wisdom teeth caused damage to other teeth?
- Is there a risk that I might have nerve damage?
- What other dental treatments might I need at a later date?
- How long does it take to completely heal and return to normal activity? our clinical team will explain to you the procedure in details and help you to make the right informed decision.
Preparing for surgery
A wisdom tooth extraction is almost always performed as an outpatient procedure in the clinic. This means that you go home the same day.
You’ll receive instructions from Picnic Point Dental Clinic dental staff on what to do before the surgery and the day of your scheduled surgery. Ask these questions:
- Will I need to make arrangements for someone to drive me home after the procedure?
- When do I need to arrive at the dental clinic or hospital?
- Do I need to avoid eating food or drinking fluids or both (fast)? If so, when do I begin?
- Can I take my prescription medications before the surgery? If so, how soon before the surgery can I take a dose?
- Should I avoid any nonprescription drugs before the surgery?
What you can expect, During the procedure?
Our clinical team may use one of three types of anesthesia, depending on the expected complexity of the wisdom tooth extraction and your comfort level. Options include:
- Local anesthesia. our clinical team administers atraumatic local anesthesia with one or more injections near the site of each extraction. Before you receive an injection, our clinical team will likely apply a substance to your gums to numb them. You’re awake during the tooth extraction. Although you’ll feel some pressure and movement, you shouldn’t experience pain.
- Sedation anesthesia. our clinical team gives you sedation anesthesia through an intravenous (IV) line in your arm or Nitrous Oxide Gas sedation. Sedation anesthesia suppresses your consciousness during the procedure. You don’t feel any pain and will have limited memory of the procedure. You’ll also receive local anesthesia to numb your gums.
- General anesthesia. In special situations, you may be offered general anesthesia. In this case our clinical team will refer you to Hospital setting to perform the procedures. You may inhale medication through your nose or have an IV line in your arm, or both. Then you lose consciousness. Your surgical team closely monitors your medication, breathing, temperature, fluids and blood pressure. You’ll experience no pain and have no memory of the procedure. Local anesthesia is also given to help with postoperative discomfort.
During wisdom tooth extraction, our clinical team:
- Makes an incision in the gum tissue to expose the tooth and bone
- Removes bone that blocks access to the tooth root
- Divides the tooth into sections if it’s easier to remove in pieces
- Removes the tooth
- Cleans the site of the removed tooth of any debris from the tooth or bone
- Stitches the wound closed to promote healing, though this isn’t always necessary
- Places gauze over the extraction site to control bleeding and to help a blood clot form.
After the procedure
If you receive sedation anesthesia or general anesthesia, you’re taken to a recovery room after the procedure. If you have local anesthesia, your brief recovery time is likely in the dental chair.
As you heal from your surgery, follow our clinical team’s instructions on:
- Bleeding. Some oozing of blood may occur the first day after wisdom tooth removal. Try to avoid excessive spitting so that you don’t dislodge the blood clot from the socket. Replace gauze over the extraction site as directed by our clinical team.
- Pain management. You may be able to manage pain with an over-the-counter pain reliever, such as (Panadol), or a prescription pain medication from your dentist or oral surgeon. Prescription pain medication may be especially helpful if bone has been removed during the procedure. Holding a cold pack against your jaw also may relieve pain.
- Swelling and bruising. Use an ice pack as directed by your dentist or surgeon. Any swelling of your cheeks usually improves in two or three days. Bruising may take several more days to resolve.
- Activity. After your surgery, plan to rest for the remainder of the day. Resume normal activities the next day, but for at least a week, avoid strenuous activity that might result in losing the blood clot from the socket.
- Beverages. Drink lots of water after the surgery. Don’t drink alcoholic, caffeinated, carbonated or hot beverages in the first 24 hours. Don’t drink with a straw for at least a week because the sucking action can dislodge the blood clot from the socket.
- Food. Eat only soft foods, such as yogurt or applesauce, for the first 24 hours. Start eating semisoft foods when you can tolerate them. Avoid hard, chewy, hot or spicy foods that might get stuck in the socket or irritate the wound.
- Cleaning your mouth. Don’t brush your teeth, rinse your mouth, spit or use mouthwash during the first 24 hours after surgery. Typically, you’ll be told to resume brushing your teeth after the first 24 hours. Be particularly gentle near the surgical wound when brushing and gently rinse your mouth with warm salt water every two hours and after meals for a week.
- Tobacco use. If you smoke, don’t do so for at least 72 hours after surgery — and wait longer than that if possible. If you chew tobacco, don’t use it for at least a week. Using tobacco products after oral surgery can delay healing and increase the risk of complications.
- Stitches. You may have stitches that dissolve within a few weeks or no stitches at all. If your stitches need to be removed, schedule an appointment to have them taken out.
When to call us?
Call our clinical team at Picnic Point Dental Clinic if you experience any of the following signs or symptoms, which could indicate an infection, nerve damage or other serious complication:
- Difficulty swallowing or breathing
- Excessive bleeding
- Fever
- Severe pain not relieved by prescribed pain medications
- Swelling that worsens after two or three days
- A bad taste in your mouth not removed with saltwater rinsing
- Pus in or oozing from the socket
- Persistent numbness or loss of feeling
- Blood or pus in nasal discharge
Results
You probably won’t need a follow-up appointment after a wisdom tooth extraction if:
- You don’t need stitches removed
- No complications arose during the procedure
- You don’t experience persistent problems, such as pain, swelling, numbness or bleeding — complications that might indicate infection, nerve damage or other problems
If complications develop, contact us to discuss treatment options.
